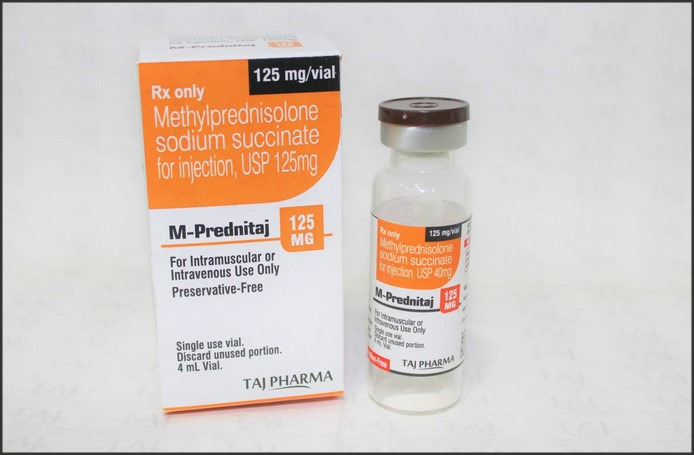
Solu Medrol 125 mg is a corticosteroid medication used to treat a variety of conditions such as allergic disorders, skin conditions, ulcerative colitis, arthritis, lupus, psoriasis, or breathing disorders. It works by decreasing the body’s immune response to these conditions, thereby reducing symptoms such as swelling, redness, and allergic-type reactions. The dosage of Solu Medrol 125 mg varies depending on the patient’s condition and response to treatment. Potential side effects may include weight gain, increased appetite, sweating, insomnia, mood changes, and digestive problems. More serious side effects can include muscle weakness, irregular heartbeats, blurred vision, and mood changes. It is important to consult with a healthcare provider before starting this medication.
Understanding Solu Medrol 125 mg: Uses, Dosage, and Potential Side Effects
Solu Medrol 125 mg, also known as Methylprednisolone, is a potent corticosteroid medication that is widely used in the medical field. It is primarily used to reduce inflammation and suppress the immune system, making it a valuable tool in the treatment of a variety of conditions. Understanding the uses, dosage, and potential side effects of Solu Medrol 125 mg is crucial for patients and healthcare providers alike.
Solu Medrol 125 mg is used in the treatment of numerous health conditions. It is often prescribed for conditions such as arthritis, lupus, severe allergic reactions, certain types of cancer, and disorders affecting the skin, kidneys, lungs, and eyes. Additionally, it is used to treat conditions that affect the nervous system, such as multiple sclerosis and certain disorders of the intestines, like ulcerative colitis. The medication works by decreasing the body’s immune response to these conditions, thereby reducing symptoms such as swelling, redness, and pain.
The dosage of Solu Medrol 125 mg varies depending on the specific condition being treated, the patient’s overall health, and their response to therapy. It is typically administered by injection into a muscle or vein as directed by a healthcare professional. The frequency of administration can range from once every other day to once every four days. It is important to follow the healthcare provider’s directions closely to ensure the medication is effective. Patients should not stop taking the medication abruptly as it can lead to withdrawal symptoms. Instead, the dosage should be gradually decreased under the supervision of a healthcare provider.
While Solu Medrol 125 mg is a powerful and effective medication, it is not without potential side effects. Common side effects include nausea, vomiting, heartburn, headache, dizziness, trouble sleeping, appetite changes, increased sweating, and acne. These side effects are generally mild and often subside as the body adjusts to the medication. However, if they persist or worsen, patients should seek immediate medical attention.
More serious side effects can occur, although they are less common. These include unusual weight gain, muscle weakness, puffy face, slow wound healing, thinning skin, bone pain, menstrual period changes, and mental/mood changes such as depression, mood swings, and anxiety. In rare cases, Solu Medrol 125 mg can cause serious, potentially fatal side effects, such as severe stomach or abdominal pain, black or tarry stools, vomit that looks like coffee grounds, and seizures. If any of these serious side effects occur, patients should seek immediate medical attention.
In conclusion, Solu Medrol 125 mg is a potent corticosteroid medication with a wide range of uses. It is effective in treating a variety of conditions by reducing inflammation and suppressing the immune system. However, it is not without potential side effects, some of which can be serious. Therefore, it is crucial for patients and healthcare providers to understand the uses, dosage, and potential side effects of Solu Medrol 125 mg to ensure safe and effective treatment.Solu Medrol 125 mg is a corticosteroid medication used to treat a variety of conditions such as allergic disorders, skin conditions, ulcerative colitis, arthritis, lupus, psoriasis, or breathing disorders. The dosage is dependent on the patient’s medical condition and response to treatment. Potential side effects can include weight gain, increased appetite, sweating, insomnia, mood changes, and digestive issues. Serious side effects are rare but can include muscle weakness, irregular heartbeat, and mood changes. It’s crucial to consult a healthcare professional before starting or stopping this medication.




 Jardiance Generic Cost: Affordable Options for Diabetes Management is a comprehensive guide that provides information about the cost-effective alternatives for managing diabetes. It focuses on the generic version of Jardiance, a popular medication used to control blood sugar levels in people with type 2 diabetes. This guide aims to help patients understand the pricing, effectiveness, and accessibility of generic Jardiance, offering a more affordable solution for diabetes management without compromising on health outcomes.
Jardiance Generic Cost: Affordable Options for Diabetes Management is a comprehensive guide that provides information about the cost-effective alternatives for managing diabetes. It focuses on the generic version of Jardiance, a popular medication used to control blood sugar levels in people with type 2 diabetes. This guide aims to help patients understand the pricing, effectiveness, and accessibility of generic Jardiance, offering a more affordable solution for diabetes management without compromising on health outcomes.