Swelling in fingers for no apparent reason is a condition that can be caused by various factors, ranging from minor injuries to serious health conditions. This condition, also known as peripheral edema, is characterized by an abnormal accumulation of fluid in the tissues of the fingers, leading to an enlarged or puffy appearance. The causes can be as simple as high salt intake, heat, or prolonged immobility, or as complex as heart, liver, or kidney diseases, arthritis, or lymphedema. Evaluation of this condition often involves a thorough medical history review, physical examination, and diagnostic tests to identify the underlying cause and determine the appropriate treatment.
Unraveling the Mystery: Fingers Swelling for No Reason – Causes and Evaluation
Swelling in fingers for no apparent reason can be a perplexing and sometimes alarming symptom. It is a condition that can cause discomfort, hinder daily activities, and raise concerns about underlying health issues. Unraveling the mystery behind this seemingly inexplicable swelling involves understanding its potential causes and the importance of proper evaluation.
The human body is a complex system, and swelling in the fingers can be a sign of various underlying conditions. One of the most common causes is edema, a condition characterized by an excessive accumulation of fluid in the body tissues. This can occur due to a variety of reasons, including heart, liver, or kidney disease, pregnancy, or certain medications. In these cases, the swelling is often not limited to the fingers but affects other parts of the body as well.
Another potential cause is arthritis, a condition that causes inflammation in the joints. Rheumatoid arthritis and osteoarthritis are the most common types that can lead to swelling in the fingers. Rheumatoid arthritis is an autoimmune disease that can cause swelling and pain in the joints, while osteoarthritis is a degenerative disease that usually affects older individuals and can cause similar symptoms.
In some cases, the swelling may be due to an injury or trauma to the hand or fingers. Even if the injury seems minor, it can lead to inflammation and swelling. Repetitive strain injuries, common in people who perform the same hand or finger movements over and over, can also cause swelling.
Allergies are another potential cause of finger swelling. This can occur as a reaction to certain foods, medications, or substances. In these cases, the swelling is usually accompanied by other symptoms such as itching, redness, or hives.
Despite these potential causes, it’s important to note that sometimes, the cause of finger swelling may not be immediately apparent. This is why proper evaluation is crucial. A healthcare professional will typically start by taking a detailed medical history and conducting a physical examination. They may ask about any recent injuries, exposure to allergens, or other symptoms that might provide clues about the cause of the swelling.
In some cases, further diagnostic tests may be necessary. These could include blood tests to check for signs of inflammation or infection, imaging tests such as X-rays or MRI to look for injuries or abnormalities in the joints, or allergy tests to identify potential allergens.
In conclusion, swelling in the fingers for no apparent reason can be a sign of various underlying conditions, from edema and arthritis to injuries and allergies. While it can be disconcerting, understanding the potential causes can help demystify this symptom. However, it’s important to seek medical attention for proper evaluation and diagnosis. This will not only help identify the cause of the swelling but also guide the appropriate treatment, ensuring that you can return to your daily activities with minimal discomfort.Swelling in fingers for no apparent reason can be caused by various factors including injury, infection, arthritis, gout, carpal tunnel syndrome, or certain medications. It can also be a symptom of more serious conditions such as heart, liver, or kidney disease. Therefore, it’s crucial to evaluate the underlying cause through a thorough medical examination, which may include blood tests, imaging studies, or other diagnostic procedures. Early diagnosis and treatment can help manage symptoms and prevent potential complications.
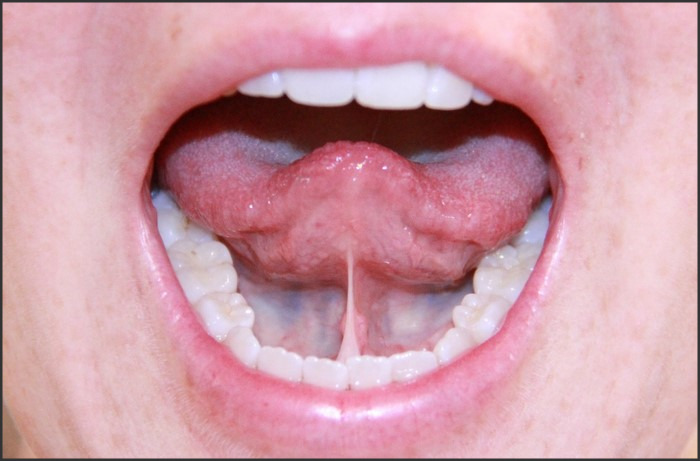
 Teeth Build-Up: Understanding Dental Procedures and Benefits is an informative guide that delves into the intricate world of dental procedures, specifically focusing on teeth build-up. This comprehensive overview provides a detailed explanation of the process, techniques, and materials used in teeth build-up procedures, as well as the benefits they offer. It aims to educate readers about the importance of dental health, the role of teeth build-up in restoring the function and aesthetics of the teeth, and how these procedures contribute to overall oral health.
Teeth Build-Up: Understanding Dental Procedures and Benefits is an informative guide that delves into the intricate world of dental procedures, specifically focusing on teeth build-up. This comprehensive overview provides a detailed explanation of the process, techniques, and materials used in teeth build-up procedures, as well as the benefits they offer. It aims to educate readers about the importance of dental health, the role of teeth build-up in restoring the function and aesthetics of the teeth, and how these procedures contribute to overall oral health.