 Torn Pec Recovery is a comprehensive guide to rehabilitation and healing after a pectoral muscle injury. It provides detailed information on the causes, diagnosis, and treatment of pectoral muscle injuries, as well as advice on how to prevent them in the future. It also offers practical tips on how to manage the pain and discomfort associated with a pectoral muscle injury, as well as how to speed up the healing process. With the help of Torn Pec Recovery, you can get back to your active lifestyle in no time.
Torn Pec Recovery is a comprehensive guide to rehabilitation and healing after a pectoral muscle injury. It provides detailed information on the causes, diagnosis, and treatment of pectoral muscle injuries, as well as advice on how to prevent them in the future. It also offers practical tips on how to manage the pain and discomfort associated with a pectoral muscle injury, as well as how to speed up the healing process. With the help of Torn Pec Recovery, you can get back to your active lifestyle in no time.
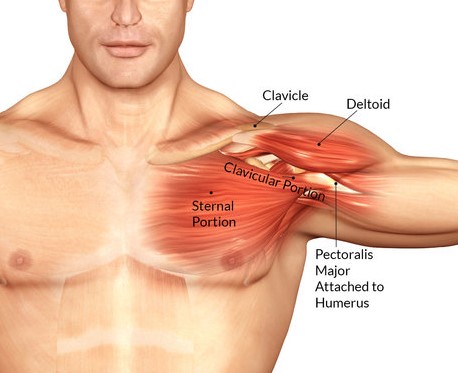
Understanding the Anatomy of the Pectoral Muscle and How to Best Recover from a Torn Pec Injury
The pectoral muscles, commonly referred to as the “pecs,” are a group of muscles located in the chest area. They are responsible for a variety of movements, including flexing the shoulder, rotating the arm, and adducting the arm. The pectoral muscles are also important for providing stability to the shoulder joint.
Unfortunately, the pectoral muscles are prone to injury, particularly tears. A torn pectoral muscle can be a very painful and debilitating injury. It is important to understand the anatomy of the pectoral muscles and the best ways to recover from a torn pectoral muscle injury.
The pectoral muscles are made up of two main muscles: the pectoralis major and the pectoralis minor. The pectoralis major is the larger of the two muscles and is responsible for most of the movement of the shoulder joint. It originates from the sternum and clavicle and inserts into the humerus. The pectoralis minor is a smaller muscle located underneath the pectoralis major. It originates from the ribs and inserts into the shoulder joint.
Tears of the pectoral muscles can occur due to a variety of causes, including overuse, trauma, or sudden force. Symptoms of a torn pectoral muscle include pain, swelling, and bruising in the chest area. It is important to seek medical attention if you suspect you have a torn pectoral muscle.
The best way to recover from a torn pectoral muscle injury is to rest and allow the muscle to heal. It is important to avoid any activities that may cause further injury or strain the muscle. Ice and anti-inflammatory medications can help reduce pain and swelling. Physical therapy can also be beneficial in helping to restore strength and range of motion.
Surgery may be necessary in some cases of a torn pectoral muscle. Surgery involves repairing the torn muscle and reattaching it to the bone. Recovery time after surgery can vary, but typically takes several weeks.
In conclusion, understanding the anatomy of the pectoral muscles and the best ways to recover from a torn pectoral muscle injury is important. Rest, ice, anti-inflammatory medications, and physical therapy are all important components of recovery. In some cases, surgery may be necessary. It is important to seek medical attention if you suspect you have a torn pectoral muscle.
Exploring the Different Treatment Options for Torn Pec Recovery and How to Choose the Right One for You
When you suffer a torn pec, it can be a difficult and painful experience. Fortunately, there are a variety of treatment options available to help you recover. It is important to understand the different treatment options and how to choose the right one for you.
The first step in treating a torn pec is to rest the affected area. This will help reduce inflammation and allow the muscle to heal. Ice and compression can also be used to reduce swelling and pain. Non-steroidal anti-inflammatory drugs (NSAIDs) may also be prescribed to reduce inflammation and pain.
Physical therapy is an important part of the recovery process. A physical therapist can help you regain strength and range of motion in the affected area. They can also provide exercises to help you regain strength and flexibility.
Surgery may be necessary in some cases. This is usually done to repair the torn muscle and reattach it to the bone. Surgery is usually recommended for severe tears that cannot be treated with other methods.
In addition to these treatments, there are also alternative therapies that may be beneficial. These include acupuncture, massage, and chiropractic care. These therapies can help reduce pain and improve mobility.
When choosing a treatment option, it is important to consider your individual needs and goals. Talk to your doctor about the best option for you. They can help you decide which treatment is best for your situation.
No matter which treatment option you choose, it is important to follow your doctor’s instructions and take the necessary steps to ensure a successful recovery. With the right treatment, you can get back to your normal activities in no time.Torn pectoral muscle injuries can be a difficult and painful experience, but with the right rehabilitation and healing techniques, a full recovery is possible. With the help of a physical therapist, a patient can develop a personalized rehabilitation plan that will help them regain strength and mobility in the affected area. Additionally, proper nutrition and rest are essential for a successful recovery. With the right approach, a patient can return to their pre-injury activities and enjoy a full and healthy life.
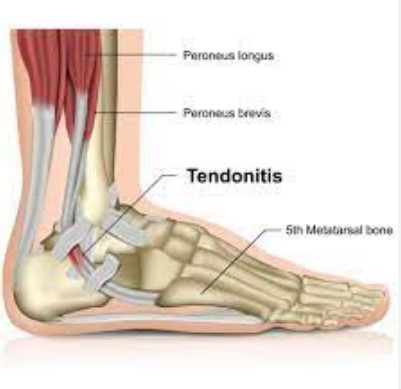 Torn ligaments in the top of the foot can be a painful and debilitating injury. The top of the foot is a complex area of the body, and the ligaments that support it can be easily damaged. Common causes of a torn ligament in the top of the foot include sports injuries, falls, and overuse. Treatment for a torn ligament in the top of the foot typically involves rest, ice, compression, and elevation. In some cases, surgery may be necessary. This article will discuss the causes of a torn ligament in the top of the foot, as well as recovery tips to help you heal quickly and safely.
Torn ligaments in the top of the foot can be a painful and debilitating injury. The top of the foot is a complex area of the body, and the ligaments that support it can be easily damaged. Common causes of a torn ligament in the top of the foot include sports injuries, falls, and overuse. Treatment for a torn ligament in the top of the foot typically involves rest, ice, compression, and elevation. In some cases, surgery may be necessary. This article will discuss the causes of a torn ligament in the top of the foot, as well as recovery tips to help you heal quickly and safely. When a loved one experiences a stroke, the journey to recovery often extends beyond the hospital stay. Providing care at home becomes essential, with unique challenges and responsibilities. Here are some important tips to guide you in offering practical and compassionate stroke recovery care in the comfort of your home.
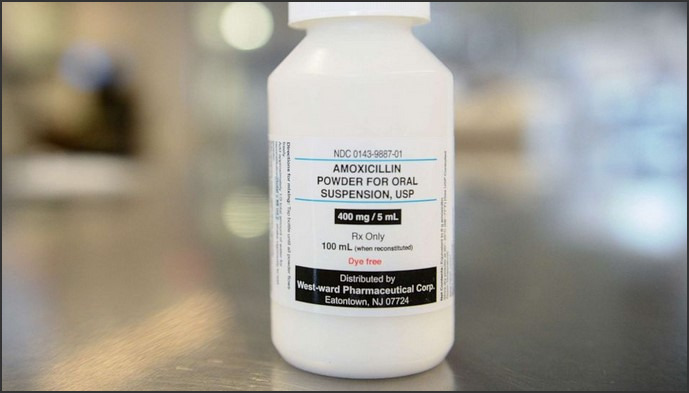
When a loved one experiences a stroke, the journey to recovery often extends beyond the hospital stay. Providing care at home becomes essential, with unique challenges and responsibilities. Here are some important tips to guide you in offering practical and compassionate stroke recovery care in the comfort of your home. Quick cold sore remedies are a great way to provide relief from the discomfort of oral herpes. Cold sores, also known as fever blisters, are caused by the herpes simplex virus and can be painful and embarrassing. Fortunately, there are a variety of remedies available that can help reduce the severity of symptoms and speed up the healing process. This article will provide an overview of some of the most effective quick cold sore remedies, including home remedies, over-the-counter medications, and prescription medications. With the right treatment, you can find relief from your cold sore symptoms and get back to feeling your best.
Quick cold sore remedies are a great way to provide relief from the discomfort of oral herpes. Cold sores, also known as fever blisters, are caused by the herpes simplex virus and can be painful and embarrassing. Fortunately, there are a variety of remedies available that can help reduce the severity of symptoms and speed up the healing process. This article will provide an overview of some of the most effective quick cold sore remedies, including home remedies, over-the-counter medications, and prescription medications. With the right treatment, you can find relief from your cold sore symptoms and get back to feeling your best.


 The American Board of Prosthodontics (ABP) is a professional organization dedicated to promoting excellence in the field of prosthodontics. Established in 1975, the ABP is the only certifying board recognized by the American Dental Association (ADA) for the specialty of prosthodontics. The ABP is committed to providing the highest standards of care for patients and to advancing the specialty of prosthodontics through rigorous credentialing and continuing education. The ABP is dedicated to promoting the highest quality of care for patients and to advancing the specialty of prosthodontics through credentialing and continuing education. The ABP is committed to providing the highest standards of care for patients and to advancing the specialty of prosthodontics through rigorous credentialing and continuing education.
The American Board of Prosthodontics (ABP) is a professional organization dedicated to promoting excellence in the field of prosthodontics. Established in 1975, the ABP is the only certifying board recognized by the American Dental Association (ADA) for the specialty of prosthodontics. The ABP is committed to providing the highest standards of care for patients and to advancing the specialty of prosthodontics through rigorous credentialing and continuing education. The ABP is dedicated to promoting the highest quality of care for patients and to advancing the specialty of prosthodontics through credentialing and continuing education. The ABP is committed to providing the highest standards of care for patients and to advancing the specialty of prosthodontics through rigorous credentialing and continuing education.
 Blood clots are a serious medical condition that can lead to life-threatening complications if left untreated. Treatment for blood clots depends on the type and severity of the clot, as well as the patient’s overall health. Medical interventions such as anticoagulant medications, thrombolytic therapy, and catheter-directed thrombolysis can be used to treat blood clots. In addition, lifestyle changes such as quitting smoking, exercising regularly, and eating a healthy diet can help reduce the risk of developing blood clots. This article will discuss the various medical interventions and lifestyle changes that can be used to treat and prevent blood clots.
Blood clots are a serious medical condition that can lead to life-threatening complications if left untreated. Treatment for blood clots depends on the type and severity of the clot, as well as the patient’s overall health. Medical interventions such as anticoagulant medications, thrombolytic therapy, and catheter-directed thrombolysis can be used to treat blood clots. In addition, lifestyle changes such as quitting smoking, exercising regularly, and eating a healthy diet can help reduce the risk of developing blood clots. This article will discuss the various medical interventions and lifestyle changes that can be used to treat and prevent blood clots.