
A podiatrist is a medical professional who specializes in the diagnosis and treatment of foot and ankle conditions. Podiatrists are also known as foot doctors, and they provide a wide range of services to help patients maintain healthy feet and ankles. These services include diagnosing and treating foot and ankle injuries, prescribing medications, performing surgery, and providing preventive care. Podiatrists also provide advice on proper foot care, such as wearing the right shoes and using orthotics. They may also provide advice on lifestyle changes that can help improve foot health. Podiatrists are an important part of the healthcare team, and they play a vital role in helping patients maintain healthy feet and ankles.
Exploring the Role of a Podiatrist: What Does a Podiatrist Do?
Podiatrists are medical professionals who specialize in the diagnosis and treatment of foot and ankle conditions. They are trained to diagnose and treat a wide range of foot and ankle problems, including bunions, hammertoes, heel pain, ingrown toenails, and plantar fasciitis. They also provide preventive care, such as regular foot exams and advice on proper foot care.
Podiatrists are trained to diagnose and treat a variety of foot and ankle conditions. They can diagnose and treat conditions such as bunions, hammertoes, heel pain, ingrown toenails, and plantar fasciitis. They can also provide preventive care, such as regular foot exams and advice on proper foot care. Podiatrists can also provide treatments such as orthotics, custom shoe inserts, and physical therapy.
In addition to diagnosing and treating foot and ankle conditions, podiatrists can also provide advice on proper foot care. This includes advice on proper footwear, exercises to strengthen the feet and ankles, and tips on how to prevent foot and ankle injuries. Podiatrists can also provide advice on how to manage chronic conditions such as diabetes and arthritis.
Podiatrists are an important part of the healthcare team. They can help patients manage their foot and ankle conditions and prevent future problems. If you have any questions or concerns about your feet or ankles, it is important to consult with a podiatrist. They can provide you with the information and treatment you need to keep your feet and ankles healthy.
Understanding the Responsibilities of a Foot Specialist: What Does a Podiatrist Do?
A podiatrist is a medical professional who specializes in the diagnosis and treatment of foot and ankle conditions. Podiatrists are highly trained and knowledgeable in the anatomy and physiology of the foot and ankle, and they are able to diagnose and treat a wide range of conditions.
Podiatrists are responsible for providing comprehensive care for the feet and ankles. This includes evaluating and diagnosing foot and ankle conditions, prescribing medications, performing surgery, and providing preventive care. Podiatrists also provide advice on proper foot care, such as wearing the right shoes and using orthotics.
Podiatrists are also responsible for educating patients about their condition and providing them with the necessary information to make informed decisions about their treatment. They may also provide referrals to other medical professionals, such as orthopedists or physical therapists, if necessary.
In addition to providing medical care, podiatrists are also responsible for providing emotional support to their patients. They may provide counseling and support to help patients cope with their condition and make lifestyle changes to improve their overall health.
Podiatrists are an important part of the healthcare team and play a vital role in helping patients maintain healthy feet and ankles. They are highly trained and knowledgeable in the diagnosis and treatment of foot and ankle conditions, and they are dedicated to providing the best possible care for their patients.In conclusion, podiatrists are highly trained medical professionals who specialize in the diagnosis, treatment, and prevention of foot and ankle conditions. They are responsible for providing comprehensive care to patients of all ages, from infants to the elderly. Podiatrists are also involved in research and education, helping to advance the field of podiatry and improve patient care. With their specialized knowledge and skills, podiatrists are essential to the health and well-being of their patients.





 Having triplets is an exciting and overwhelming experience. It can be a challenge to manage the needs of three babies at once, but it can also be incredibly rewarding. Triplets bring a unique set of joys and challenges that can be difficult to navigate. From the initial shock of the news to the daily juggling of three babies, parents of triplets must be prepared for the unique demands of raising multiples. With the right support and resources, parents can find ways to make the experience of having triplets a positive and rewarding one.
Having triplets is an exciting and overwhelming experience. It can be a challenge to manage the needs of three babies at once, but it can also be incredibly rewarding. Triplets bring a unique set of joys and challenges that can be difficult to navigate. From the initial shock of the news to the daily juggling of three babies, parents of triplets must be prepared for the unique demands of raising multiples. With the right support and resources, parents can find ways to make the experience of having triplets a positive and rewarding one. Mushrooms are a type of fungi that have been used for centuries in traditional medicine and cuisine. They are a versatile and nutritious food that can be used in a variety of dishes. Not only are they delicious, but they also offer a range of health benefits and nutritional value. Mushrooms are a great source of vitamins, minerals, and antioxidants, and they can help to boost the immune system, reduce inflammation, and even fight cancer. In addition, they are low in calories and fat, making them a great addition to any healthy diet. In this article, we will explore the health benefits and nutritional value of mushrooms, as well as some tips for incorporating them into your diet.
Mushrooms are a type of fungi that have been used for centuries in traditional medicine and cuisine. They are a versatile and nutritious food that can be used in a variety of dishes. Not only are they delicious, but they also offer a range of health benefits and nutritional value. Mushrooms are a great source of vitamins, minerals, and antioxidants, and they can help to boost the immune system, reduce inflammation, and even fight cancer. In addition, they are low in calories and fat, making them a great addition to any healthy diet. In this article, we will explore the health benefits and nutritional value of mushrooms, as well as some tips for incorporating them into your diet. Eating for Your Blood Type: Exploring the Blood Type Diet is a comprehensive guide to understanding the connection between your blood type and the foods you eat. It provides an in-depth look at the science behind the Blood Type Diet, as well as practical advice on how to make dietary changes to improve your health and well-being. This book is an invaluable resource for anyone interested in learning more about the Blood Type Diet and how it can help them achieve their health goals.
Eating for Your Blood Type: Exploring the Blood Type Diet is a comprehensive guide to understanding the connection between your blood type and the foods you eat. It provides an in-depth look at the science behind the Blood Type Diet, as well as practical advice on how to make dietary changes to improve your health and well-being. This book is an invaluable resource for anyone interested in learning more about the Blood Type Diet and how it can help them achieve their health goals. Clear wire braces are a discreet and comfortable option for orthodontic treatment. They are made of clear plastic and are virtually invisible when worn. Clear wire braces are a great choice for those who want to improve their smile without the hassle of traditional metal braces. They are also more comfortable than metal braces, as they are less likely to cause irritation to the gums and cheeks. Clear wire braces are a great way to get the smile you want without the hassle of traditional braces.
Clear wire braces are a discreet and comfortable option for orthodontic treatment. They are made of clear plastic and are virtually invisible when worn. Clear wire braces are a great choice for those who want to improve their smile without the hassle of traditional metal braces. They are also more comfortable than metal braces, as they are less likely to cause irritation to the gums and cheeks. Clear wire braces are a great way to get the smile you want without the hassle of traditional braces.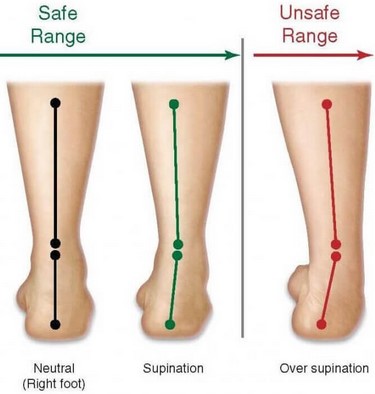 Supination of the foot is a gait abnormality that can cause a variety of issues for those affected. It is a condition in which the foot rolls outward when walking or running, resulting in an increased pressure on the outside of the foot and ankle. This can lead to pain, instability, and an increased risk of injury. Understanding the causes and treatments of supination of the foot can help those affected manage their condition and reduce their risk of injury.
Supination of the foot is a gait abnormality that can cause a variety of issues for those affected. It is a condition in which the foot rolls outward when walking or running, resulting in an increased pressure on the outside of the foot and ankle. This can lead to pain, instability, and an increased risk of injury. Understanding the causes and treatments of supination of the foot can help those affected manage their condition and reduce their risk of injury. Painful pectoral muscle is a condition that affects the chest muscles, causing pain and discomfort. It can be caused by a variety of factors, including overuse, injury, or medical conditions. Symptoms of painful pectoral muscle can include pain in the chest, difficulty breathing, and difficulty moving the arms. Treatment for painful pectoral muscle typically involves rest, physical therapy, and medications. Recovery strategies may include stretching, strengthening exercises, and lifestyle modifications. This article will discuss the causes, symptoms, and recovery strategies for painful pectoral muscle.
Painful pectoral muscle is a condition that affects the chest muscles, causing pain and discomfort. It can be caused by a variety of factors, including overuse, injury, or medical conditions. Symptoms of painful pectoral muscle can include pain in the chest, difficulty breathing, and difficulty moving the arms. Treatment for painful pectoral muscle typically involves rest, physical therapy, and medications. Recovery strategies may include stretching, strengthening exercises, and lifestyle modifications. This article will discuss the causes, symptoms, and recovery strategies for painful pectoral muscle. Orthodontic spacers are an important part of the process of preparing for braces. They are small rubber bands or metal rings that are placed between the teeth to create a small gap. This gap is necessary for the braces to be properly fitted and for the teeth to be moved into the desired position. Orthodontic spacers are typically used in conjunction with other orthodontic treatments such as braces, retainers, and headgear. They are an important part of the process of achieving a beautiful, healthy smile.
Orthodontic spacers are an important part of the process of preparing for braces. They are small rubber bands or metal rings that are placed between the teeth to create a small gap. This gap is necessary for the braces to be properly fitted and for the teeth to be moved into the desired position. Orthodontic spacers are typically used in conjunction with other orthodontic treatments such as braces, retainers, and headgear. They are an important part of the process of achieving a beautiful, healthy smile. Swollen knuckles can be a painful and uncomfortable condition that can affect anyone at any age. It is caused by a variety of factors, including injury, arthritis, and infection. Treatment for swollen knuckles depends on the underlying cause, but may include rest, ice, compression, and elevation. In some cases, medications or surgery may be necessary. It is important to seek medical attention if the swelling does not improve or if it is accompanied by other symptoms. This article will discuss the causes, treatment, and when to see a doctor for swollen knuckles.
Swollen knuckles can be a painful and uncomfortable condition that can affect anyone at any age. It is caused by a variety of factors, including injury, arthritis, and infection. Treatment for swollen knuckles depends on the underlying cause, but may include rest, ice, compression, and elevation. In some cases, medications or surgery may be necessary. It is important to seek medical attention if the swelling does not improve or if it is accompanied by other symptoms. This article will discuss the causes, treatment, and when to see a doctor for swollen knuckles.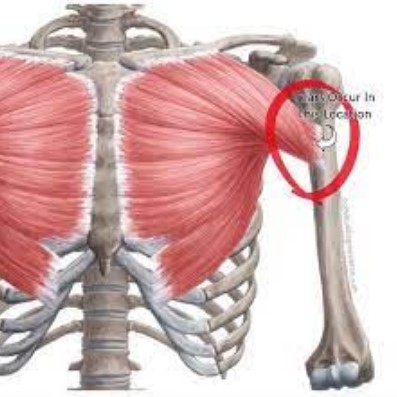 A torn pectoral muscle is a serious injury that can cause significant pain and disability. It is most commonly seen in athletes who participate in activities that involve pushing or pulling motions, such as weightlifting, football, and wrestling. The pectoral muscle is a large muscle located in the chest that helps to move the arm and shoulder. When it is torn, it can cause pain, swelling, and difficulty moving the arm. Treatment for a torn pectoral muscle typically involves rest, physical therapy, and possibly surgery. This article will discuss the causes, symptoms, and recovery strategies for a torn pectoral muscle.
A torn pectoral muscle is a serious injury that can cause significant pain and disability. It is most commonly seen in athletes who participate in activities that involve pushing or pulling motions, such as weightlifting, football, and wrestling. The pectoral muscle is a large muscle located in the chest that helps to move the arm and shoulder. When it is torn, it can cause pain, swelling, and difficulty moving the arm. Treatment for a torn pectoral muscle typically involves rest, physical therapy, and possibly surgery. This article will discuss the causes, symptoms, and recovery strategies for a torn pectoral muscle.